How To Improve Call Light Response Time
- Enquiry commodity
- Open Access
- Published:
Perspectives of staff nurses of the reasons for and the nature of patient-initiated telephone call lights: an exploratory survey study in four United states hospitals
BMC Health Services Research volume 10, Article number:52 (2010) Cite this article
Abstract
Background
Little research has been done on patient call light use and staff response fourth dimension, which were found to be associated with inpatient falls and satisfaction. Nurses' perspectives may moderate or mediate the aforementioned relationships. This exploratory report intended to understand staff'south perspectives about call lights, staff responsiveness, and the reasons for and the nature of phone call light apply. It as well explored differences among hospitals and identified significant predictors of the nature of phone call calorie-free use.
Methods
This cross-exclusive, multihospital survey written report was conducted from September 2008 to January 2009 in four hospitals located in the Midwestern region of the The states. A brief survey was used. All 2309 licensed and unlicensed nursing staff members who provide direct patient care in 27 adult care units were invited to participate. A full of 808 completed surveys were retrieved for an overall response rate of 35%. The SPSS 16.0 Window version was used. Descriptive and binary logistic regression analyses were conducted.
Results
The principal reasons for patient-initiated calls were for toileting help, pain medication, and intravenous problems. Toileting assistance was the leading reason. Each staff responded to half dozen to 7 calls per hour and a call was answered within 4 minutes (estimated). 49% of staff perceived that patient-initiated calls mattered to patient safety. 77% agreed that that these calls were meaningful. 52% thought that these calls required the attention of nursing staff. 53% thought that answering calls prevented them from doing the disquisitional aspects of their part. Staff'southward perceptions near the nature of calls varied across hospitals. Junior staff tended to overlook the importance of answering calls. A nurse participant tended to perceive calls as more likely requiring nursing staff's attention than a nurse aide participant.
Conclusions
If answering calls was a loftier priority amid nursing tasks, staff would perceive calls equally being important, requiring nursing staff's attention, and being meaningful. Therefore, answering calls should not be perceived as preventing staff from doing the critical aspects of their part. Additional efforts are necessary to reach the ideal or even a reasonable level of patient safety-first practice in current hospital environments.
Groundwork
Patient call light usage and nurse responsiveness to telephone call lights are two intertwined concepts that could pertain to patients' safety during hospital stays [one, two]. Still, picayune research has been done on this topic. In general, patient- or family-initiated telephone call calorie-free usage is associated with how often patients or family visitors have unmet needs and require assistance. Response time to call lights is primarily determined by the nurses' reaction to each call light and may be linked to the circumstances present when a call is initiated.
Note that the present system of hospital intendance is based on the supposition that patients are able to get help past activating their nurse telephone call arrangement (also called call calorie-free or call bong). However, cognitive impairment, visual loss, and decreased mobility could make it difficult for patients to utilize the nurse call system when they need assist. Inability to phone call for help (e.g., the call lite panel or button is non within attain) may effect in hospital-acquired damage (e.g., falling out of the bed due to un-assisted transfer) [3]. A study [4] identified multiple extrinsic risk factors for falls related to human involvement including: difficulties in determining patient care priorities, nursing staff's misconception nigh the purpose of telephone call lights, call lights not being answered in a timely manner, difficulty in implementing timed ascertainment and toileting plans, and patient assignments not existence in shut proximity, which may delay the responses to patients' call lights and needs. In a study related to autumn prevention efforts [5], recently discharged older patients emphasized that nurses should provide assist and respond a call lite in a timely manner and a major safety concern during hospital stays was lack of availability of nurses to help when needed.
In addition, two studies [1, 2] found that more calls for help were related to less fall-related patient injuries per 1000 patient-days and longer telephone call lite response times. When the boilerplate response time to phone call lights was longer, the patient satisfaction scores were lower [ane]. A recent written report [6] also examined the correlation betwixt the patient satisfaction at discharge in relation to the number of the call light requests from the patient's room and staff response time in a 32-bed surgical unit of measurement. However, no statistically significant relationships were found. It's arguable that nurses' perspectives virtually patient-initiated call lights may moderate or mediate the relationships amid patient call light usage, nurse call light responsiveness, and patient satisfaction with nursing care.
The nurse call arrangement and problems relevant to nursing practice
The phone call light is a vital patient communication link during hospital stays and is actually i of the few means by which cognitively intact patients can do some meaningful command over their care. The commonly adopted nurse call arrangement features have the ability of allowing unit of measurement clerks to receive and screen patient calls in the nurses' station, which is meant to reduce unnecessary nurse interruptions. Such features may save actual nursing time, and enable some nurses to begin preparing to meet patients' needs earlier entering their rooms. Bug with the commonly adopted nurse call organisation are, for example: inability to locate the nurse, inability to prioritize and confirm calls, and disability to speak straight to patients and staff [vii].
Call light technology has continued to develop (e.m., Vocera integration with a nurse call organization). Enhanced nurse telephone call systems accept sought to provide more than a means for beckoning nursing personnel to the patient'due south room and to significantly increment their functionality. Although these advances provide improvements for workflow and offer an opportunity to better response times, none of these systems have been shown to meliorate efficiencies, patient prophylactic or reduce costs [8–x].
Hospitalized patients spend most of their time in their room necessitating utilize of call lights to have their needs met. Previous studies [11–xiv] have identified possible reasons why patients and families use call lights, including (but not limited to): (1) urgent calls, (ii) toileting assistance, (iii) intravenous problems, (4) pain medication, (v) repositioning and transfer aid, (half-dozen) personal assistance (e.m., for food, water), (7) obtaining information, (8) getting nurses' attention, (9) asking for nursing staff'southward companionship, and (10) accidentally pushing the call light.
Information technology is ordinarily assumed that if a nurse responds to a call light more than chop-chop, the patient may accept less opportunity to fall. All the same, phone call lights are perceived by some nurses equally mere dissonance and an interruption to nursing tasks, instead of an important way for patients to request assistance [12]. Deitrick and assembly [11] examined problems related to answering patient call lights in astute inpatient care settings and found that the most frequent comments of patients were: (i) delays in getting phone call lights answered, (2) variation in the call light response time from a low of less than a minute to a high of twenty minutes, (3) the amount of fourth dimension it took to handle the patient's request once the light was answered, and (4) the patient's asking non beingness fulfilled once the telephone call calorie-free was answered. Frustration over delays in answering call lights is 1 of the most frequent comments that patients make.
In short, little research has been washed on patient call lite use and staff call light response time, and only ane modest-calibration pilot study [15] intended to understand how nursing staff view patient-initiated call lights. This pilot written report [15] found that, although the bulk of the staff (81.6%) agreed that call lights were meaningful, only half of the staff members perceived that call lights mattered to patient safe and required nursing staff attention and 44% idea that answering telephone call lights prevented them from doing critical aspects of their role.
Theoretical framework
The National Quality Forum (NQF) [xvi] suggested issue, procedure, structure, and patient-centered measures as considerations for supporting internal healthcare organisation quality improvement. Using NQF's approach for falls' assessment, the outcome measures include: (ane) falls with injuries, and (2) falls prevalence. The procedure measures intend to quantify the level of staff adherence to organizational policy that represents effective falls prevention practices, including: (1) pct of patients screened for falls, and (2) per centum of patients educated most fall prevention strategies and risks. The structure measures include: (one) the presence of an organizational falls prevention policy, and (2) the presence of measurable structures in place to ensure accountability for performance. The patient-centered measures refer to show that patients' values and preferences are respected.
Previous studies [4, sixteen–eighteen] suggested that intrinsic (those integral to the patient) and extrinsic (those external to the patient) risk factors for fall and injurious fall occurrence tin be interwoven with each other causing an fifty-fifty greater risk together than separately. The intrinsic risk factors are composed of, but not limited to, patients' demographics, cognitive functioning, functioning status, physiologic status, principal patient medical condition, vigil level, length of stay, and telephone call light usage. The extrinsic risk factors include, but are not express to, risks related to environment (east.thousand., design of effects and equipments, patient-staff communication devices), treatment and medications, staffing, use of unlicensed personnel (e.g., sitters, family visitors), and nursing actions to address patient needs (e.thousand., staff response time to patient needs, fall prevention protocol).
Figure 1 was developed to illustrate the significance of this written report within the context of patient prophylactic with a focus on inpatient falls. This effigy used a macro-view to describe the importance of this subject area. Staff's response time to phone call lights was categorized as a staff-centered process measure and patient call light utilize charge per unit was a patient-centered process factor. It was assumed that nurses' perspectives about phone call lights may moderate or mediate the relationships among patient call light usage, nurse responsiveness, and patient satisfaction. Consequently, this project was proposed to explore nurses' viewpoints.
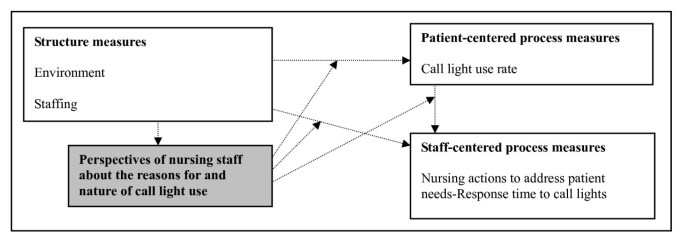
The conceptual model of this study. This study explored the perspectives of nursing staff almost the reasons for and the nature of telephone call light employ; it did non exam the relationships betwixt the variables in the boxes.
Purpose of this study and research questions
This exploratory, cross-sectional, multihospital survey study attempted to understand staff's perspectives well-nigh patient-initiated telephone call lights, staff responsiveness, and the reasons for and nature of call lite use. Information technology also explored the differences in the perspectives of staff members in 4 hospitals. In addition, information technology was designed to identify pregnant predictors of the nature of call low-cal use. Every bit an exploratory study, the candidate predictors included: infirmary, staff'southward age, tenure, gender, job title, educational groundwork, unit blazon, and principal working shift. These were limited to the indicators collected in the survey as a study limitation. To stand for to the study purposes, this study answered five research questions:
- (1)
What were the reasons for telephone call lights as perceived past staff members?
- (2)
How many call lights per hour did a staff member respond to alone?
- (three)
How long did it take to reply a call low-cal during the day, evening, and dark shifts?
- (4)
How did a staff member perceive the nature of phone call lights?
- (5)
What were the significant predictors for staff'southward perspectives about the nature of call lights?
Methods
Pattern
This exploratory, cross-sectional, multihospital survey study was conducted from September 2008 to Jan 2009 at four hospitals located in the Midwestern region of the United States. The written report was approved by each hospital's institutional review lath and the writer's employer university (HUM22711). There was no disharmonize of interest.
Sample and setting
A user-friendly sample was used, due to express upkeep, and simply four astute hospitals were recruited to participate in this study, including a total of 27 adult inpatient acute care units. The numbers of study units and bed size for each respective study infirmary were: Hospital 1, an academic medical center (12 units, bed size about 900); Hospital 2, a community pedagogy infirmary (iv units, bed size about 300); Hospital three, a veteran affairs medical center (3 units, bed size about 100); and Hospital 4, a instruction medical centre (8 units, bed size virtually 700). All these 27 report units have a nurse call organisation in place. In social club to maximize the number of the completed surveys, all 2309 licensed and unlicensed nursing staff members who provide direct patient intendance in the study adult care units, equally the targeted population, were invited to participate.
Instrumentation and data drove
The call light staff survey questionnaire (sixteen items of the nurse self-reported measures) used in this paper has been airplane pilot tested in a regime hospital [fifteen] (Table one and Additional file 1). These items were composed based on the previous studies [eleven–14] and adult for the purpose of this multihospital written report. This survey has content validity; nine clinical experts reviewed each item for appropriateness and word use. Unfortunately, content validity indexes on the experts' comments were not performed. Equally a effect of the experts' comments, only the employ of words in the survey was modified for increased clarity. This survey was previously pre-tested for clarity and fourth dimension/ease of completion by 38 staff nurses and nurse aides, who worked in an acute medical-surgical unit at a Michigan academic medical center. No changes were fabricated based on the outcomes of the pre-test and pilot test. Because all the questions are single-particular scales, a reliability analysis was non conducted [15].
The items used to measure out the studied concepts included: staff's perspectives nearly patient-initiated call lights (Item ix), staff responsiveness (Item 11), the reasons for telephone call light utilise (Detail eight), and the nature of phone call calorie-free utilize (Items 12-fifteen). The candidate predictors of the nature of call light utilise included infirmary (documented by the writer), staff'south historic period (Item two), tenure (Item 7), gender (Detail 1), job title (Detail five), educational groundwork (Particular 3), unit of measurement type (Item 4), and primary working shift (Item six). Specifically, for the responses nerveless within Item viii (the reasons for telephone call light use), the indicated prevalence (in percentage) was then ranked among the identified situations inside each completed survey and recoded for further data assay (one = The most prevalent reason). Each participant may assign two or more than two of the selected reasons the same frequency/prevalence level. As a issue, two or more than ii of the selected reasons may be ranked as the virtually prevalent reason inside a completed survey.
The survey packages were left in each potential participant's mailbox located in the staff lounge. Staff participants received a copy of the survey questionnaire and an information canvas about this study. Participation was voluntary and anonymous, with no identifiers recorded or tracked on the survey questionnaire. Render of the completed surveys indicated consent. To prompt completion, a reminder follow-up letter of the alphabet was sent to all possible participants 2 weeks afterwards the survey was disseminated.
Data analyses
The Statistical Package for the Social Sciences (16.0 Window version; SPSS Inc., Chicago, IL, USA) was used for data analyses. Descriptive analyses were used to answer the showtime iv enquiry questions. To answer the fifth question, four binary logistic regression models were developed to determine significant predictors (blastoff was set up at .05) of 4 dependent variables respectively, including: (one) important to patients' condom, (2) requiring nursing staff's attention, (3) reasons for call lights existence meaningful, and (4) action of answering telephone call lights preventing staff from doing critical aspects of their part. Candidate predictors (hospital, staff member's historic period, tenure, gender, chore title, educational background, unit type, and primary working shift) were entered into the models at the same time. Dummy variables were created for the categorical variables (hospital, gender, job title, educational background, unit blazon, and primary working shift); the number of created dummy variables for each categorical variable was: the number of categories minus 1. It resulted in a total of 17 predicators in each regression model. The responses of all participants (nursing staff and nurse aides) were included in the analyses.
Results
A total of 808 completed surveys were retrieved from a full of 27 adult inpatient astute intendance units at iv hospitals for an overall response rate of 35%. The numbers of valid surveys for each corresponding study hospital were: Hospital i, an academic medical eye (northward = 459); Infirmary 2, a customs teaching hospital (n = 119); Hospital 3, a veteran affairs medical center (north = 47); and Hospital four, a teaching medical heart (north = 183). Amidst these participants, 636 (79%) staff nurses (registered nurses and licensed applied nurses) and 172 (21%) nurse aides returned the completed surveys report.
For the unabridged group of participants, Pearson χ 2 tests showed meaning associations betwixt hospitals and the proportions of participants' highest completed education level, work title, unit type, and primary working shift. Ane-way ANOVA tests found pregnant differences in the participants' hateful historic period and tenure in years across four written report hospitals; the staff participants from Hospital 3 had the highest mean in age (hateful = 44.57 years) and those from Hospital 2 had the longest hateful in tenure (mean = nine.94 years) (Table two). The post-obit sub-sections presented the answers to the specific research questions by the theme of the inquiry question.
Reasons for call light use
Based on all the respondents, amongst the 10 mentioned possibilities, the reasons identified by at least xc% of the participants for call lite use were: (1) hurting medication and management (the well-nigh often identified reason), (2) bathroom assistance, (3) intravenous problems or pump alert, (4) personal assistance, (five) accidental pressing of the call light, and (6) repositioning or transfer (Table three).
Based on the frequency of each identified reason being ranked as the almost prevalent reason within each respondent, the reason for bath assistance was near oft identified equally the leading reason for call calorie-free use, followed past need for pain medication and management, and intravenous problems or pump alert. In other words, staff members most ofttimes identified bathroom help as the most common reason for call light employ (Tabular array three).
Number of call lite responded by staff
Based on staff'south recall, on average, each staff fellow member responded to 6.46 calls per hour, ranging from 4.80 calls (Infirmary 3) to 6.83 calls (Hospital i). In other words, each staff may reply to about 52 calls during an viii-hour shift or 78 calls during a 12-60 minutes shift (virtually one call every 9 minutes). No significant differences were plant beyond the 4 hospitals in the means of the number of calls per hour to which an individual staff person responded (Table four).
Response time to call lights
The average length of time to answer a phone call light was three.57 minutes during 24-hour interval shifts, three.70 minutes during evening shifts, and 3.42 minutes during dark shifts. Overall, regardless of unlike shifts, a phone call was expected to exist answered with 4 minutes or iii minutes and 42 seconds. No significant differences were noted across the iv hospitals in the means of the cocky-reported response time to call lights (Table four).
Nature of call lights
A little less than one-half of the participants (due north = 373, 49%) perceived that call lights mattered to patient safe, 406 (52%) idea call lights required nursing staff attending, 604 (77%) considered them meaningful, and 480 (53%) thought that answering call lights prevented them from doing critical aspects of their role. Pearson χtwo tests showed significant differences between hospitals on staff's perceptions about call lite importance to patients' safety and on staff's perception that answering call lights prevented them from doing critical aspects of their office (Table iii).
Predicting the perceived nature of call lights
The results of iv logistic regression models were presented in Table 5. The perceptions of all participants (nursing staff and nurse aides) were included in the analyses. The dependent variables for these four regression models were: (1) important to patients' rubber, (2) requiring nursing staff's attention, (iii) reasons for telephone call lights being meaningful, and (4) activity of answering call lights preventing staff from doing critical aspects of their role. Candidate predictors (infirmary, staff member'south historic period, tenure, gender, job championship, educational groundwork, unit type, and primary working shift) were entered into the models at the same fourth dimension. Dummy variables were created for the categorical variables (infirmary, gender, job title, educational groundwork, unit blazon, and master working shift). A full of 17 candidate predicators were entered into each regression model.
The first binary logistic regression model with the dependent variable of call lights being of import to patients' safety showed that only the chiselled variable of hospital was a significant predictor, where a staff member, who worked in Hospital i or Hospital 2 would perceive call lights as being less important to patients' safety. In other words, only ane significant predictor was identified (Table 5).
The second binary logistic regression model with the dependent variable of phone call lights requiring nursing staff's attention indicated that a nurse participant tended to perceive call lights as more likely to crave nursing staff's attention than a nurse aide participant. In addition, the categorical variable of the respondent's principal working shift was a significant predictor; however, none of the shifts predicted the dependent variable (Tabular array 5).
The third binary logistic regression model with the dependent variable of the reasons for phone call lights being meaningful showed that the chiselled variable of the hospital was a significant predictor, where a staff member, who worked in Hospital ane or Hospital 2, would perceive call lights as being less meaningful. If participants had longer tenure, they tended to perceive phone call lights as being more meaningful. The categorical variable of the respondent's primary working shift was a significant predictor, where a staff member, who worked in the day shift or 12-hour night shift, would perceive call lights as being less meaningful (Table 5).
The quaternary binary logistic regression model with the dependent variable of the action of answering call lights preventing the staff participants from doing critical aspects of their function showed that the categorical variable of the hospital was a significant predictor, where staff members, who worked in Infirmary 1 or Hospital ii, tended to perceive that the action of answering call lights would prevent them from doing disquisitional aspects of their role. The categorical variable of the respondent'south primary working shift was a significant predictor, where staff members, who worked on the 12-hour day shift, tended to perceive that the activity of answering call lights would prevent them from doing critical aspects of their role (Table 5).
Discussion
This exploratory, cross-sectional, multihospital survey report attempted to empathize staff'southward perspectives about patient-initiated call lights, staff responsiveness, and the reasons for and the nature of call light use. Information technology also determined the predictors of the nature of telephone call light apply, including these 4 dependent variables: (1) important to patients' safety, (2) requiring nursing staff's attention, (3) reasons for telephone call lights existence meaningful, and (4) action of answering call lights preventing staff from doing critical aspects of their function. The post-obit sub-sections discussed the answers to the specific research questions by the theme of the research question.
Reasons for call light utilize
The respond to the first research question suggested that the primary vi reasons for patient-initiated phone call lights were: (1) pain medication and management, as the most often identified reason, (2) bath aid, (3) intravenous problems or pump alert, (4) personal aid, (5) accidental pressing of the phone call low-cal, and (half dozen) repositioning or transfer. Toileting assistance was the leading reason for call lite use. These findings suggested that if a infirmary included rounding for patient comfort and safety [12, 19] every bit 1 of the patient safety initiatives, such rounding should be oriented to patients' toileting needs, pain management, and intravenous problems (specified requests).
When targeting on a patient's specified requests, personal assistance (unspecified, orderly requests) may exist addressed at the aforementioned time. The reason is that specified requests are more predictable and tend to require licensed nurses' attention than the unspecified ones, such as needs for water and reposition [20]. This written report'due south findings also implied that licensed nurses should exist the principal person responding to call lights.
In addition, the rounding schedule should be justified based on the frequency of each individual patient's needs and changes in medical conditions (e.g., post-operation). For example, an private patient's toileting needs may vary over the entire course of hospitalization, due to changes in medication usage (e.grand., diuretics, benzodiazepines, sedatives) and changes in dependency in transferring/mobility (e.yard., postoperatively).
Patient call light use and nurse responsiveness
The answers associated with the 2nd and third research questions suggested that, on boilerplate, each staff member responded to 6 to 7 telephone call lights per hour. The estimated length of time to respond a call light was inside 4 minutes. It should be noted that the survey questionnaire did non inquire participants to specify the number of calls they responded to and did not ask participants their response time to call lights based on the nature or types of call lights.
In near of the inpatient intendance settings, patient- or family-initiated call lights have been categorized into normal calls (made from the pillow speaker), urgent calls (when a normal call was non answered within 3 minutes, an urgent call will be sent out), or toileting or bathroom calls (the calls made from the bath). Few institutions have adopted newer pillow speaker applied science, where patients can specify their needs past pushing the button for water, pain medication, or bathroom/bedpan assistance.
To endorse patient-centered care, nursing executives and unit of measurement managers must promote the effectiveness of patient-initiated call lite utilize and the efficiency of staff'due south responsiveness to phone call lights. As a practical thing, upgrading the call calorie-free arrangement engineering science is necessary to assistance nursing staff determine patient care priorities for the purpose of reducing patient injury and falls [20]. For example, the call light panel could have three options to bespeak the urgency level of each patient- or family-initiated call: (1) urgent call (east.g., unexpected bleeding, shortness of breath, dizziness), (2) normal phone call (e.g., bath assistance, intravenous issues or pump warning, pain medication and direction), and (3) orderly aid (e.g., repositioning, transfer or mobility assistance, personal help, obtaining information most medications and health condition, enervating a nurse's companionship at bedside) [20].
Nature of telephone call lights
The answer to the fourth research question suggested that less than half (49%) of the participants perceived that patient-initiated call lights mattered to patient safety. Surprisingly, 77% of them agreed that that these calls were meaningful. In addition, but 52% thought that these calls required the attention of nursing staff. Consequently, information technology seems to be legitimate that up to 53% of the participants idea that answering call lights prevented them from doing the disquisitional aspects of their part.
It was causeless that if answering call lights was prioritized higher amid nursing tasks, a staff member would perceive telephone call lights equally being of import to patient safety, requiring nursing staff'due south attending, and meaningful. If so, the action of answering call lights should not be perceived as preventing staff members from doing the disquisitional aspects of their role.
Appropriately, it is suggested that regular on-the-job grooming of patient prophylactic-outset practices with a focus on addressing patients' call lights would exist required to enhance the consensus perception of the importance levels of each telephone call lite amid staff members. Such educational interventions should besides target improving the morale of staff members past acknowledging their efforts to promote patient safety. It is also essential to develop a simple, straightforward, feedback loop to staff on their operation from patients, families, and unit managers (east.chiliad., quality of patient-nurse interaction, patients' need being addressed in a timely style). Occasionally, incentives to staff would exist needed to reinforce patient prophylactic-starting time practices. Such incentives may be linked to the feedback mechanism.
Predicting the perceived nature of call lights
The answers to the fifth research question suggested that if staff members worked in Infirmary 1 or Hospital 2, they would tend to perceive telephone call lights every bit being less important to patients' safety, every bit being less meaningful, and that the action of answering call lights would prevent them from doing disquisitional aspects of the nursing role. In other words, staff's perceptions about the nature of call lights were found to vary significantly beyond hospitals. This difference tin be due to the organization's patient safety civilisation or the leadership profiles of the hospital or nursing executives and heart-level and unit of measurement-level managers. However, this study did not mensurate the study hospitals' patient safety civilisation or leadership profiles, and is unable to test the same possible relationship.
Tenure was found to be a meaning predictor of the reasons for telephone call lights existence meaningful. If a participant had longer tenure, he or she tended to perceived phone call lights as being more meaningful. This finding suggested that inferior staff tended to overlook the importance of answering patient- or family-initiated call lights. Therefore, new staff orientation should include information related to patient prophylactic-first exercise with a focus on addressing patients' call lights.
In addition, a nurse participant tended to perceive call lights as more likely requiring nursing staff'due south attention than a nurse aide participant. Consequently, on-the-job training for patient safety-outset practices should be tailored for nurse aides to be consistent with their roles in the process of delivering patient care. It may be advisable to offering unlike patient safe-beginning do on-the-job training sessions for nurses and nurse aides to address their specific requirements.
Also, staff members who worked a 12-hour 24-hour interval shift tended to perceive that the activity of answering telephone call lights would preclude them from performing critical aspects of their role. It is possible that the day shift has more procedures, treatments, admissions, or discharges that a nurse or nurse adjutant must handle than those working in evening and night shifts. The respondent'south primary working shift was also a pregnant predictor of the reasons for call lights existence meaningful. Withal, the predicting direction of the respondent'south primary working shift was not conclusive, and further research is needed.
In short, the candidate predictors of hospital, tenure, chore title, and primary working shift were found to affect at least one of the four dependent variables of the nature of telephone call light use. The candidate predictors of staff member'due south historic period, gender, educational background, and unit type were not found to be significant predictors affecting any of the four dependent variables of the nature of call light usage.
These findings suggested that employment-related characteristics (infirmary, tenure, job championship, and main working shift) were significant determinants of nurses' perceptions virtually the nature of telephone call light use. The predictor of hospital could exist a dominant characteristic that supersede the influence of unit type. The findings likewise suggested that individual staff'due south characteristics (historic period, gender, and educational groundwork) should not be considered as candidate predictors in predicting nurses' perceptions on the issues related to the nature of call light apply. The perceived nature of telephone call light employ could be a shared, hospital-broad phenomenon that may be linked to an arrangement's culture, instead of each individual staff's demographic characteristics.
Study limitations and future research directions
The telescopic of this study is limited to 4 hospitals located in the Midwestern region of the The states, reducing the power to generalize the findings. In add-on, each hospital adopted similar only somewhat different call light-related devices or technology (eastward.g., when a call went off, the responsible staff was informed via a personal pager versus wireless phone). Each infirmary has somewhat unlike mechanisms and focuses on monitoring patient safe initiatives (e.g., fall prevention protocols, regular rounding for patient condolement and safety). Nonetheless, no study has systematically investigated the differences of the result of adopting unlike call light-related devices on patient safety outcomes.
In an attempt to minimize the length of time to complete the staff surveys, a limited number of questions were included. The reliability and validity information nearly this survey is limited, including threats to internal validity. Farther instrument development is needed to develop items that inquire about the tasks that need to exist handled by a nurse versus an adjutant as the almost appropriate helper, and the perceived urgency level of each phone call light utilise reason. As well, it could be helpful to use focus groups to solicit nurses' and patients' opinions.
The researcher recognized that additional factors may also exist disquisitional to staff's response fourth dimension to call lights, including the efficiency of teamwork among a patient'south responsible staff members, staff's priority among their assigned tasks, patients' vigil levels, and changes in a patient's physical status and mental condition. However, these issues are not addressed in this paper equally study limitations. In improver, since patient self-reported outcomes regarding call light usage and responsiveness (e.m. consumer assessment, inpatient satisfaction) could not be used to show its concordance with the results of the nurse self-reported measures used in this report, it is a study limitation. This limitation should exist taken into account for future research directions.
Future studies should consider including homo resource factors in the assay of the perceived nature of patient- and family unit-initiated call lights, including staffing patterns (e.thou., total nursing hours per patient day by different shifts) and skill mix (due east.g., the registered nurse/unlicensed nursing personnel ratio, the usage rate of sitters). Pressing research focuses include investigating the relationships of staff'south perceptions nearly the nature of telephone call lights with NQF-endorsed® upshot measures (e.g., falls prevalence, falls with injuries), mail-discharge patient satisfaction scores (east.k., the Infirmary Consumer Assessment of Healthcare Providers and Systems, also known every bit HCAHPS; the monthly inpatient satisfaction survey questionnaire), and the call light utilize and responsiveness information recorded from the patient room phone call low-cal tracking system (e.g., Responder® Iv, manufactured by Rauland: http://www.rauland.com/ResponderIV.cfm). In addition, it would be essential to link staff's perceived nature of call lights with patient satisfaction and clinical outcome indicators, and to explore and develop cause-and-effect relationships between these variables, if whatsoever. It is also crucial to examine the characteristics of the patients for whom the nurses provide intendance and its differences across hospitals.
Conclusions
It was assumed that if answering call lights was more than highly prioritized amid nursing tasks, a staff member would perceive telephone call lights as beingness important to patient rubber, requiring nursing staff's attention, and being meaningful. If then, the action of answering telephone call lights should not be perceived equally preventing staff members from doing the critical aspects of their role. However, this multihospital study institute that merely 49% of the participants perceived that patient-initiated call lights mattered to patient condom, just 52% idea that these calls required the attention of nursing staff, and upwardly to 53% of the participants thought that answering call lights prevented them from doing the disquisitional aspects of their role.
Obviously, boosted efforts are necessary to reach the platonic or even a reasonable level of patient condom-commencement practice in current hospital environments. To endorse patient-centered care, nursing executives and unit managers must promote the effectiveness of patient-initiated call low-cal use and the efficiency of staff'south responsiveness to phone call lights. Regular on-the-chore preparation of patient safety-beginning practices with a focus on addressing patients' call lights would be required to heighten consensus on and sensation of the perceived important levels of call lights among staff members.
References
-
Tzeng HM, Yin CY: Do call light use and response time contribute to inpatient falls and inpatient dissatisfaction?. J Nurs Care Qual. 2009, 24 (iii): 232-242.
-
Tzeng HM, Yin CY: Relationship betwixt call light use and response time and inpatient falls in acute intendance settings. J Clin Nurs. 2009, 18 (23): 3333-3341. 10.1111/j.1365-2702.2009.02916.10.
-
Duffy S, Mallery L, Gordon J, Carver D: Ability of hospitalized older adults to employ their call bong: A pilot study in a tertiary care teaching hospital. Aging Clin Exp Res. 2005, 17 (5): 390-393.
-
Tzeng HM, Yin CY: The extrinsic risk factors for inpatient falls in hospital patient rooms. J Nurs Intendance Qual. 2008, 23 (3): 233-241.
-
Tzeng HM, Yin CY: Perspectives of recently discharged patients on hospital fall-prevention programs. J Nurs Care Qual. 2009, 24 (ane): 42-49.
-
Roszell Due south, Jones CB, Lynn MR: Call bell requests, call bell response time, and patient satisfaction. J Nurs Care Qual. 2009, 24 (1): 69-75.
-
Miller ET, Deets C, Miller RV: Nurse call systems: impact on nursing performance. J Nurs Care Qual. 1997, 11 (3): 36-43.
-
ECRI: Enhanced nurse call systems. Health Devices. 2001, 30 (4): 102-146.
-
Kuruzovich J, Angst CM, Faraj S, Agarwal R: Wireless communication role in patient response time: A study of Vocera integration with a nurse telephone call system. Comput Inform Nurs. 2008, 26 (3): 159-166. x.1097/01.NCN.0000304780.27070.ee.
-
Taylor DP, Coakley A, Reardon Thousand, Kuperman GJ: An assay of inpatient nursing communications needs. Stud Health Technol Inform. 2004, 107 (2): 1393-1397.
-
Deitrick L, Bokovoy J, Stern G, Panik A: Trip the light fantastic toe of the telephone call bells: Using ethnography to evaluate patient satisfaction with quality of intendance. J Nurs Care Qual. 2006, 12 (iv): 316-324.
-
Meade CM, Bursell AL, Ketelsen L: Effects of nursing rounds on patients' call light use, satisfaction, and rubber. Am J Nurs. 2006, 106 (nine): 58-70.
-
Van Handel K, Krug B: Prevalence and nature of telephone call calorie-free requests on an orthopedic unit. Orthop Nurs. 1994, 13 (one): 13-20. 10.1097/00006416-199401000-00006.
-
Torres SM: Rapid-wheel process reduces patient telephone call bell use, improves patient satisfaction, and anticipates patient'southward needs. J Nurs Adm. 2007, 27 (11): 480-482.
-
Tzeng HM: Perspectives of staff nurses toward patient- and family unit-initiated call light usage and response fourth dimension to call lights. Appl Nurs Res. 2009.
-
National Quality Forum (NQF): Rubber Practices for Amend Healthcare-2009 Update: A Consensus Written report. 2009, Washington, DC: National Quality Forum
-
Currie 50: Fall and injury prevention. Patient Condom and Quality: An Evidence-Based Handbook for Nurse (AHRQ Publication No. 08-0043). Edited by: Hughes RG. 2008, Rockville, Dr.: Agency for Healthcare Research and Quality, United states Department of Health and Man Services, 195-250.
-
Joint Commission: Defining the problem of falls. Reducing the Risk of Falls in Your Health Care Organisation. Edited past: Smith IJ. 2005, Oakbrook Terrace, IL: Joint Commission, thirteen-27.
-
Quigley PA, Hahm B, Collazo S, Gibson West, Janzen S, Powell-Cope Thousand, Rice F, Sarduy I, Tyndall K, White SV: Reducing serious injury from falls in two veterans' hospital medical-surgical units. J Nurs Care Qual. 2009, 24 (1): 33-41.
-
Tzeng HM, Schneider TE: Answering the call: Upgrading call lite system technology can help nursing staff determine patient intendance priorities to reduce patient injury and falls. Advance for Nurses. 2009, April 8: [http://nursing.advanceweb.com/Article/Answering-the-Call-10.aspx?prg=21]
Pre-publication history
-
The pre-publication history for this newspaper can be accessed here:http://www.biomedcentral.com/1472-6963/10/52/prepub
Acknowledgements
This study was partially supported by the 2009 Midwest Nursing Research Guild Seed Research Grant.
Author data
Authors and Affiliations
Corresponding author
Additional data
Competing interests
The author declares that she has no competing interests.
Authors' contributions
THM for the entire projection.
Electronic supplementary material
Authors' original submitted files for images
Rights and permissions
This article is published nether license to BioMed Central Ltd. This is an Open Access article distributed nether the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and Permissions
Nigh this article
Cite this article
Tzeng, HM. Perspectives of staff nurses of the reasons for and the nature of patient-initiated call lights: an exploratory survey study in four USA hospitals. BMC Wellness Serv Res 10, 52 (2010). https://doi.org/10.1186/1472-6963-10-52
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/1472-6963-10-52
Keywords
- Staff Fellow member
- Binary Logistic Regression Model
- Unit of measurement Type
- Candidate Predictor
- Patient Prophylactic Civilization
Source: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-10-52

0 Response to "How To Improve Call Light Response Time"
Post a Comment